Addiction is a complex and multifaceted issue that extends far beyond illicit substances, affecting individuals from all walks of life. From the potent grip of opioids to everyday foods we consume without a second thought, understanding addiction requires exploring both neurological mechanisms and environmental influences.
This article delves into the science behind substance dependency, highlighting why certain drugs—particularly opioids—are so dangerously addictive, how quickly dependence can develop, and what alternatives exist for managing pain safely. Additionally, it examines street drugs’ risks and uncovers surprising parallels between drug addiction and our relationship with highly processed sugary foods.

GreatLife Isn’t Just a Program—It’s Your Launchpad to Lasting Success.
1. Identifying the Most Addictive Drug: A Closer Look at Substance Dependency
Determining the most addictive drug involves examining multiple factors, including physical dependence, psychological cravings, withdrawal severity, and overall impact on an individual’s life. While substances such as cocaine, heroin, methamphetamine, and nicotine are frequently cited among the most addictive drugs globally, research consistently highlights opioids—particularly heroin—as one of the strongest contenders due to their profound effects on brain chemistry.
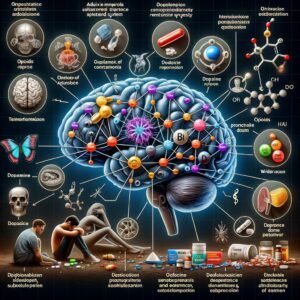
Opioids function by binding to opioid receptors in the brain’s reward centers and pain pathways. This interaction triggers a powerful release of dopamine—a neurotransmitter associated with pleasure and reinforcement—which significantly heightens feelings of euphoria. The rapid onset of these pleasurable sensations reinforces repeated use patterns that quickly escalate into dependency.
Heroin exemplifies this dynamic clearly; its potency combined with rapid absorption into the bloodstream creates intense euphoric experiences unmatched by many other substances. Consequently, users often find themselves trapped in cycles of compulsive use despite severe negative consequences affecting health, relationships, employment status, or legal standing.
However, addiction potential is not solely defined by physiological responses but also influenced heavily by environmental circumstances and individual vulnerabilities—including genetic predisposition or mental health conditions like anxiety or depression—that can amplify susceptibility to substance abuse disorders.

Take Control of Your Wellness and Wealth—Start Your GreatLife Today.
2. Why Are Opioids So Highly Addictive? Unveiling the Science Behind Their Power
Opioids exert their powerful addictive potential primarily through their interaction with the brain’s reward system, specifically targeting opioid receptors located throughout the central nervous system. These receptors regulate pain perception and emotional responses, making opioids highly effective for pain relief but also significantly increasing addiction risk. When opioids bind to these receptors, they trigger a surge of dopamine—a neurotransmitter associated with pleasure and reward—creating an intense sense of euphoria that reinforces repeated use.
Repeated exposure to opioids leads to neuroadaptation, a process in which the brain adjusts its chemistry and structure in response to continuous drug presence. Over time, this adaptation diminishes natural dopamine production and receptor sensitivity, compelling individuals to increase dosage or frequency of use to achieve similar pleasurable effects—a phenomenon known as tolerance. As tolerance develops further, physical dependence emerges; users experience withdrawal symptoms such as anxiety, nausea, muscle aches, insomnia, and severe cravings when attempting cessation.
Moreover, opioids affect areas of the brain responsible for decision-making and impulse control—primarily within regions like the prefrontal cortex—which impairs judgment regarding drug-seeking behaviors despite adverse consequences. This neurological alteration contributes substantially toward compulsive substance abuse patterns characteristic of opioid addiction.
Additionally significant is genetic predisposition: specific individuals possess genetic variations influencing how effectively their bodies metabolize opioids or respond neurologically upon initial exposure. Environmental factors—including stress levels or previous trauma—also play significant roles by heightening vulnerability toward developing dependency following opioid usage.
Collectively understanding these biological mechanisms clarifies why opioids carry such profound addictive potential compared with other substances commonly used medicinally or recreationally today.

Turn Aspirations Into Achievements—One Click Starts It All.
3. Ranking Opioids by Addiction Potential: Which One Tops the List?
When evaluating opioids based on their addiction potential, several factors come into play, including potency, duration of effect, and how quickly they cross the blood-brain barrier. At the top of this list is heroin, a semi-synthetic opioid derived from morphine.
Heroin’s rapid onset and intense euphoric effects significantly increase its addictive potential; users often report developing dependence after only a few uses due to its powerful impact on brain chemistry.
Following closely behind heroin is fentanyl, an extremely potent synthetic opioid approximately 50 to 100 times stronger than morphine. Its high potency means even small doses can produce profound euphoria and sedation—factors that greatly enhance its addictive qualities. Fentanyl’s widespread presence in illicit drug markets has contributed substantially to overdose deaths worldwide.
Oxycodone ranks third in terms of addiction risk among commonly prescribed opioids. Often marketed under brand names such as OxyContin or Percocet, oxycodone provides effective pain relief but carries significant risks for misuse due to its strong euphoric properties when taken at higher-than-prescribed doses or through alternative routes like crushing tablets for inhalation or injection.
Hydrocodone (Vicodin) and morphine also present considerable addiction risks but typically rank slightly lower compared to heroin, fentanyl, and oxycodone because their slower onset reduces immediate reinforcement effects associated with rapid highs.
Ultimately, while all opioids carry inherent risks for dependency and abuse potential due to their pharmacological nature affecting reward pathways in the brain, heroin remains consistently recognized as having the highest overall addiction liability among these substances.
4. How Quickly Can Someone Become Addicted to Opioids? The Timeline Explained
The timeline for opioid addiction varies significantly depending on several factors, including dosage, frequency of use, individual physiology, and the specific type of opioid consumed. However, research indicates that dependence can develop alarmingly quickly, often within days or weeks of regular usage. Prescription opioids such as oxycodone or hydrocodone may lead to physical dependence in as little as five days when taken consistently at therapeutic doses prescribed by medical professionals.
Initially, users experience relief from pain and a sense of euphoria due to opioids’ interaction with the brain’s reward centers. This pleasurable sensation reinforces continued use and accelerates the development of tolerance, a condition where higher doses are required over time to achieve similar effects. As tolerance grows rapidly, individuals often escalate their intake without fully recognizing the emerging signs of dependency.
Within two weeks to one month of consistent opioid consumption—even under medically supervised conditions—users commonly report withdrawal symptoms upon cessation or reduction in dosage. These withdrawal symptoms include anxiety, muscle aches, insomnia, nausea, and intense cravings for more opioids; these unpleasant sensations further perpetuate ongoing drug-seeking behavior.
Moreover, psychological addiction can manifest even sooner than physical dependence because it is driven by emotional reliance on opioids for stress relief or coping mechanisms rather than purely physiological needs alone. Consequently, some individuals may exhibit addictive behaviors after only a few exposures.
Ultimately, while timelines vary individually based on genetics and environmental influences among other factors, the rapid onset potential underscores why healthcare providers emphasize caution when prescribing opioids and advocate vigilant monitoring throughout treatment periods.

Start Small, Dream Big—GreatLife Helps You Build It.
5. Pain Relief Without Risk: Non-Addictive Alternatives for Managing Pain
Managing pain effectively without the risk of addiction is a critical consideration in healthcare today, especially given the widespread concerns surrounding opioid dependency. Fortunately, several non-addictive alternatives exist that provide significant relief while minimizing potential harm. One prominent option includes nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and naproxen, which can effectively reduce inflammation and alleviate mild to moderate pain without causing dependence.
Additionally, physical therapy has emerged as an essential component in managing chronic pain conditions. Through targeted exercises and manual techniques, physical therapists help patients strengthen muscles, improve mobility, and decrease discomfort over time.
Complementary therapies, such as acupuncture, have also gained recognition for their ability to stimulate the body’s natural pain-relieving mechanisms by promoting the release of endorphins and improving circulation.
Moreover, cognitive-behavioral therapy (CBT) offers psychological strategies aimed at changing negative thought patterns associated with chronic pain perception. By addressing emotional responses to discomfort through coping skills training and stress management techniques, CBT enables individuals to manage their symptoms more effectively on their own.
Innovative technologies, such as transcutaneous electrical nerve stimulation (TENS) units, provide another viable alternative by delivering low-voltage electrical currents directly to the affected areas of the skin surface. This method helps disrupt pain signals traveling along nerves while simultaneously stimulating endorphin production, offering effective short-term relief without addictive side effects.
Ultimately, adopting a multidisciplinary approach combining medication-free treatments alongside lifestyle modifications—including regular exercise routines or mindfulness practices—can significantly enhance quality-of-life outcomes for those experiencing persistent or acute episodes of discomfort while safeguarding against addiction risks inherent in traditional pharmacological interventions.
Say Yes to Health, Wealth, and Purpose—Join the GreatLife Revolution.
6. Street Drugs and Addiction Risks: What Substance Holds the Highest Danger?
When examining street drugs, understanding their addiction potential and associated risks is crucial for effective prevention and treatment strategies. Among illicit substances, heroin consistently emerges as one of the most dangerous due to its profound addictive properties and severe health consequences. Derived from morphine, heroin rapidly crosses the blood-brain barrier upon administration, producing an intense euphoric sensation that significantly increases its addictive potential.
Heroin’s potency lies in its ability to bind swiftly to opioid receptors in the brain, creating immediate feelings of pleasure followed by a powerful craving once the effects diminish. This rapid cycle reinforces compulsive use patterns that escalate quickly into dependence. Additionally, frequent heroin use leads users toward increased tolerance levels—requiring larger doses to achieve similar effects—and heightens overdose risk substantially.
Beyond physiological dangers such as respiratory depression leading potentially to fatal overdoses, intravenous heroin use also carries significant secondary risks, including transmission of infectious diseases like HIV/AIDS or hepatitis through shared needles. Furthermore, street-purchased heroin often contains adulterants such as fentanyl—a synthetic opioid exponentially more potent than morphine—which dramatically amplifies overdose fatalities.
While other street drugs like methamphetamine or cocaine present substantial addiction concerns themselves due to their stimulant properties and psychological dependency factors, respectively, none match heroin’s lethal combination of physical dependence severity coupled with high mortality rates stemming directly from usage practices and unpredictable purity levels found on illicit markets today.
Consequently, among common street substances available illegally worldwide today, heroin remains uniquely positioned at peak danger regarding both addiction likelihood and overall harm inflicted upon individuals who engage regularly with this perilous drug.
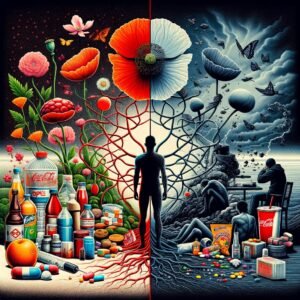
7. Beyond Drugs—What’s the World’s Most Addictive Food and Why?
When examining addictive foods, sugar consistently emerges as one of the most habit-forming substances worldwide. Scientific research indicates that sugar activates reward pathways in the brain similar to those triggered by addictive drugs, such as opioids or cocaine. This activation releases dopamine, a neurotransmitter associated with pleasure and reinforcement of behaviors, thereby creating cravings and compulsive consumption patterns.
Foods high in refined sugars—such as candies, pastries, soft drinks, and processed snacks—are engineered to maximize palatability through precise combinations of sweetness, texture, and flavor intensity.
These hyper-palatable characteristics can override the body’s natural satiety signals within its regulatory systems. Consequently, individuals often consume these products beyond their nutritional needs or in response to hunger cues.
Additionally, regular intake of sugary foods contributes to tolerance development; over time, individuals require increasingly larger amounts to achieve comparable levels of satisfaction. Withdrawal symptoms, including irritability, fatigue, headaches, or intense cravings, may also occur when attempting to reduce sugar intake abruptly.
Moreover, accessibility plays a significant role in food addiction prevalence. Sugary products are widely available globally at affordable prices across various socioeconomic contexts, a factor further reinforcing habitual consumption patterns among diverse populations.
Understanding why sugar-rich foods hold such powerful addictive potential involves recognizing both biological mechanisms within our neurological reward system and external factors, such as product formulation strategies employed by manufacturers aiming for repeat consumer engagement.
Recognizing this dynamic enables healthcare professionals to gain a deeper understanding of dietary interventions aimed at reducing dependency on highly processed, sugary items while promoting healthier eating habits overall.
Level Up Your Life with Proven Wellness and Financial Strategies—Act Now!
Conclusion:
Recognizing the intricate nature of addiction—from potent opioids like heroin to seemingly harmless yet highly addictive sugary foods—is essential in addressing this global health challenge effectively. By gaining deeper insights into how substances interact with our brain chemistry and identifying factors contributing to their addictive potential, we become better equipped to prevent dependency before it begins.
Embracing non-addictive pain management strategies, along with mindful dietary choices, can significantly reduce the risk while promoting overall well-being. Ultimately, awareness combined with proactive measures provides a strong foundation for combating addiction across its many forms, ensuring healthier lives for individuals worldwide.